Virtual Reality Nature Scenes Found to Ease Chronic Pain, Study Shows
Immersive 360° Landscapes Reduce Pain Sensitivity by Activating the Brain’s Natural Pain-control Systems

A new wave of research suggests you don’t need a forest outside your window to tap nature’s pain-soothing power—you can put it on. In July 2025, University of Exeter scientists reported that spending time in immersive virtual-reality (VR) nature scenes significantly ease the development and spread of chronic pain sensitivity in the lab, and that the effect was strongest when people truly felt “present” in the virtual environment.
The peer-reviewed paper, published in PAIN, used both careful pain testing and brain imaging to unpack why this works.
What the new study found

Researchers induced sensitization in the nervous system of 30 healthy adults using a standard high-frequency stimulation model, which reliably mimics features of long-term, neuropathic-like pain. Participants then experienced one of three conditions: a 45-minute 360° VR nature session (waterfalls in Oregon), the same footage on a regular 2D screen, or no intervention.
Only the immersive VR condition meaningfully reduced the development and spread of mechanical secondary hyperalgesia (a hallmark of sensitized pain processing), and the benefit persisted through the end of the session. Crucially, relief scaled with “presence”—the stronger the feeling of being in nature, the greater the analgesia.
University summaries note that immersive VR nature was roughly twice as effective as 2D video at reducing pain experience, and that reductions in pain-related sensitivity were still evident at least five minutes after the session. For people who can’t easily access green spaces—like many living with chronic conditions—this matters: VR can deliver a therapeutically rich “dose” of nature on demand.
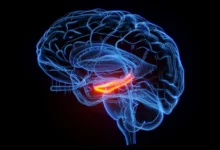
How it may work in the brain
The researchers also tested brain activity with MRI scans while participants experienced pain from a cold gel. They found that watching nature in VR changed how certain brain regions ‘talked’ to each other. Specifically, it seemed to help the brain’s natural pain-control system kick in, so fewer pain signals spread through the nervous system.
The effect was strongest when people really felt like they were inside the virtual nature scene, which suggests that the sense of presence helps the brain turn down pain more effectively.
The Exeter work builds on a broader line of evidence that nature exposure—virtual or real—tempers pain. Earlier in 2025, a Nature Communications study showed that simply watching well-designed nature videos lowered both reported pain and brain activity tied to pain processing compared with urban or indoor scenes. The authors argued this wasn’t placebo; the brain’s nociceptive (pain-signal) pathways were genuinely less reactive.
VR isn’t a magic bullet, but it is becoming a legitimate tool in multimodal pain management. In 2021, the U.S. FDA authorized the first at-home VR therapeutic for chronic low-back pain—a program grounded in behavioral skills rather than nature content—after randomized trials showed meaningful, durable benefits.
The regulatory milestone signaled that immersive, non-drug approaches can cross the bar for safety and effectiveness. Nature-based VR adds another, potentially complementary, path: it leans on our hard-wired response to natural environments to turn down pain signaling—with minimal side effects.
What this means for people with chronic pain
For clinics, hospitals, and care homes—places where stepping outside isn’t always feasible—curated VR nature sessions could offer accessible, low-risk relief and pair easily with physical therapy, CBT, or medications.
The practical takeaways from the new study are straightforward: aim for immersive, high-quality 360° nature content; run sessions long enough to let presence build (the study used ~45 minutes); and measure outcomes beyond immediate distraction, since benefits persisted.
The PAIN trial simulated chronic-like sensitization in healthy volunteers; it didn’t test people diagnosed with chronic pain, and the sample was small.
We still need large, real-world trials in specific conditions (e.g., neuropathic pain, fibromyalgia), dose-finding work (how often, how long), and comparisons across different natural environments and personalization levels. But taken together with the 2025 neuroimaging results and past VR analgesia research, the case for “virtual nature as therapy” is getting stronger.
[Source]